Long-term safety and efficacy of ozanimod in relapsing multiple sclerosis in DAYBREAK: an open-label extension study of ozanimod phase 1−3 trials
Abstract
Background:
Ozanimod, an oral sphingosine 1-phosphate receptor 1 and 5 modulator, is approved in the US and EU for treatment of relapsing multiple sclerosis (RMS).
Methods:
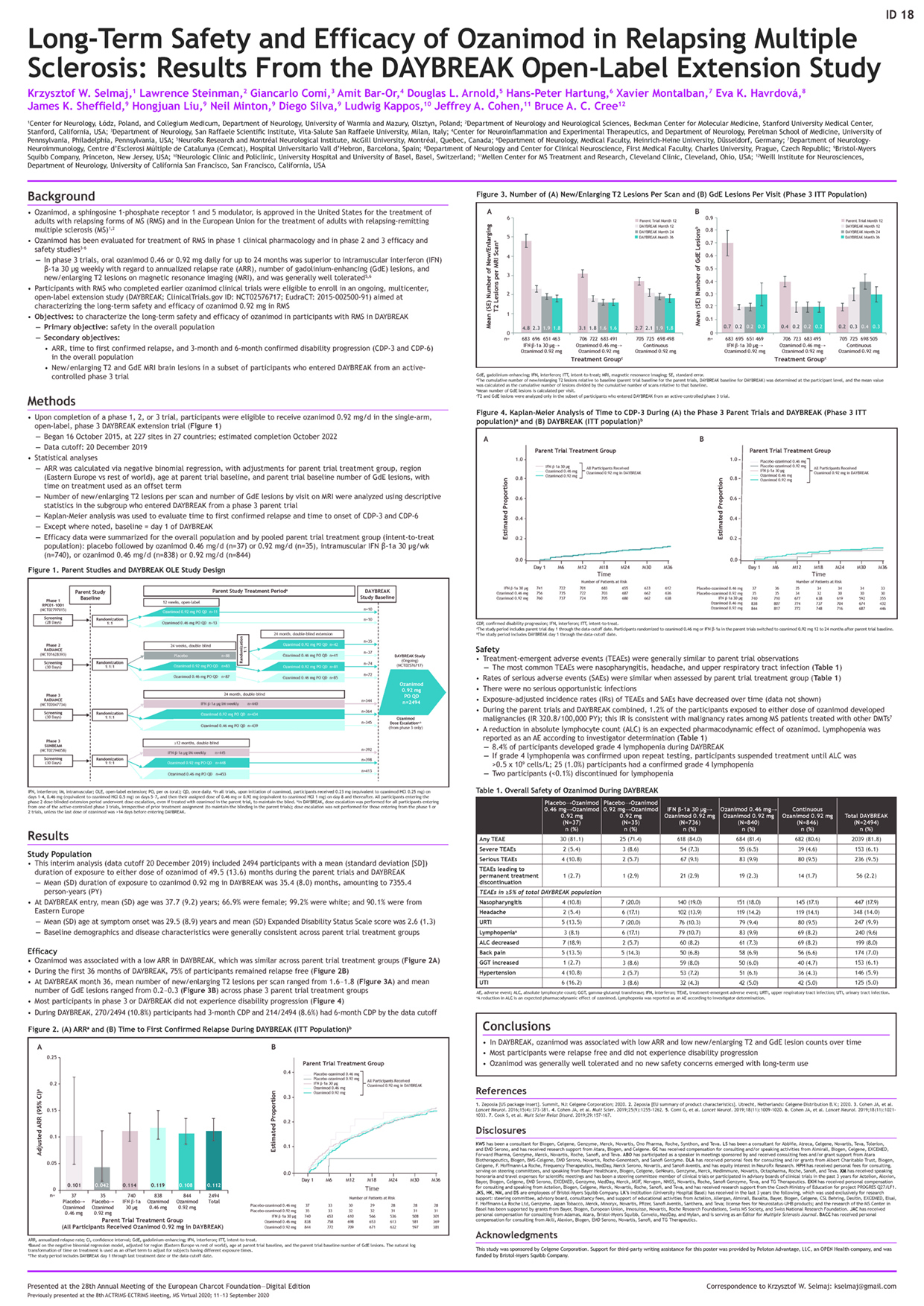
RMS participants who completed a phase 1–3 ozanimod trial were eligible for DAYBREAK (NCT02576717), an ongoing open-label extension (OLE) trial of ozanimod 0.92 mg/d (equivalent to ozanimod HCl 1 mg). The primary objective was to evaluate safety. Efficacy was evaluated with annualized relapse rate (ARR), calculated via European Charcot Foundation 2020 3001 Safety and Efficacy Page 2 of 2 negative binomial regression and pooled for all parent-trial treatment groups.
Number of new/enlarging T2 and gadolinium-enhancing (GdE) MRI brain lesions were reported for those who entered the OLE from a phase 3 parent trial.
Results:
This interim analysis (data cut 20 December 2019; presented at ACTRIMS-ECTRIMS 2020) included 2494 participants with mean (range) ozanimod exposure of 35.4 (0.03–50.2) months in the OLE. Adjusted ARR in the OLE was 0.112 (95% CI, 0.093‒0.135). At months 24 and 36, 79% and 75% of participants, respectively, were relapse free in the OLE. Three- and 6-month confirmed disability progression was observed in 10.8% and 8.6% of OLE participants, respectively. At 24 months, mean number of new/enlarging T2 lesions per scan was similar across parent-trial treatment groups (range, 1.57–1.90), as was mean number of GdE lesions (0.2‒0.4). In the OLE, 2039 participants (81.8%) had treatment-emergent adverse events (TEAEs), and 236 (9.5%) had serious TEAEs (SAEs). These rates were similar across parent-trial treatment groups. The most common TEAEs were nasopharyngitis (17.9%), headache (14%), upper respiratory tract infection (9.9%), and lymphopenia (9.6%). There were no serious opportunistic infections. Exposure-adjusted TEAE and SAE incidence rates have decreased over time.
Conclusions:
Ozanimod was associated with low ARR and new/enlarging T2 and GdE lesion counts. Most participants were relapse free and did not experience disability progression. No new safety concerns emerged with long-term use.