Characteristics of a population-based multiple sclerosis cohort treated with disease-modifying drugs in a universal healthcare setting
Abstract
Background:
Relatively little is known about the use of disease-modifying drugs (DMDs) for multiple sclerosis (MS) in the population-based universal healthcare setting. We described the characteristics of a population-based cohort with MS and their DMD exposure in four Canadian provinces (British Columbia, Saskatchewan, Manitoba and Nova Scotia).
Methods:
We identified all adults (aged ≥18 years) with MS using linked population-based health administrative data. Individuals were followed from the most recent of their first MS or demyelinating event or 01/January/1996 (study entry), to the earliest of death, emigration, or study end (up to 31/March/2018) and use of the MS DMDs was described. Cohort characteristics examined included sex, age, socioeconomic status, and comorbidity burden.
Results:
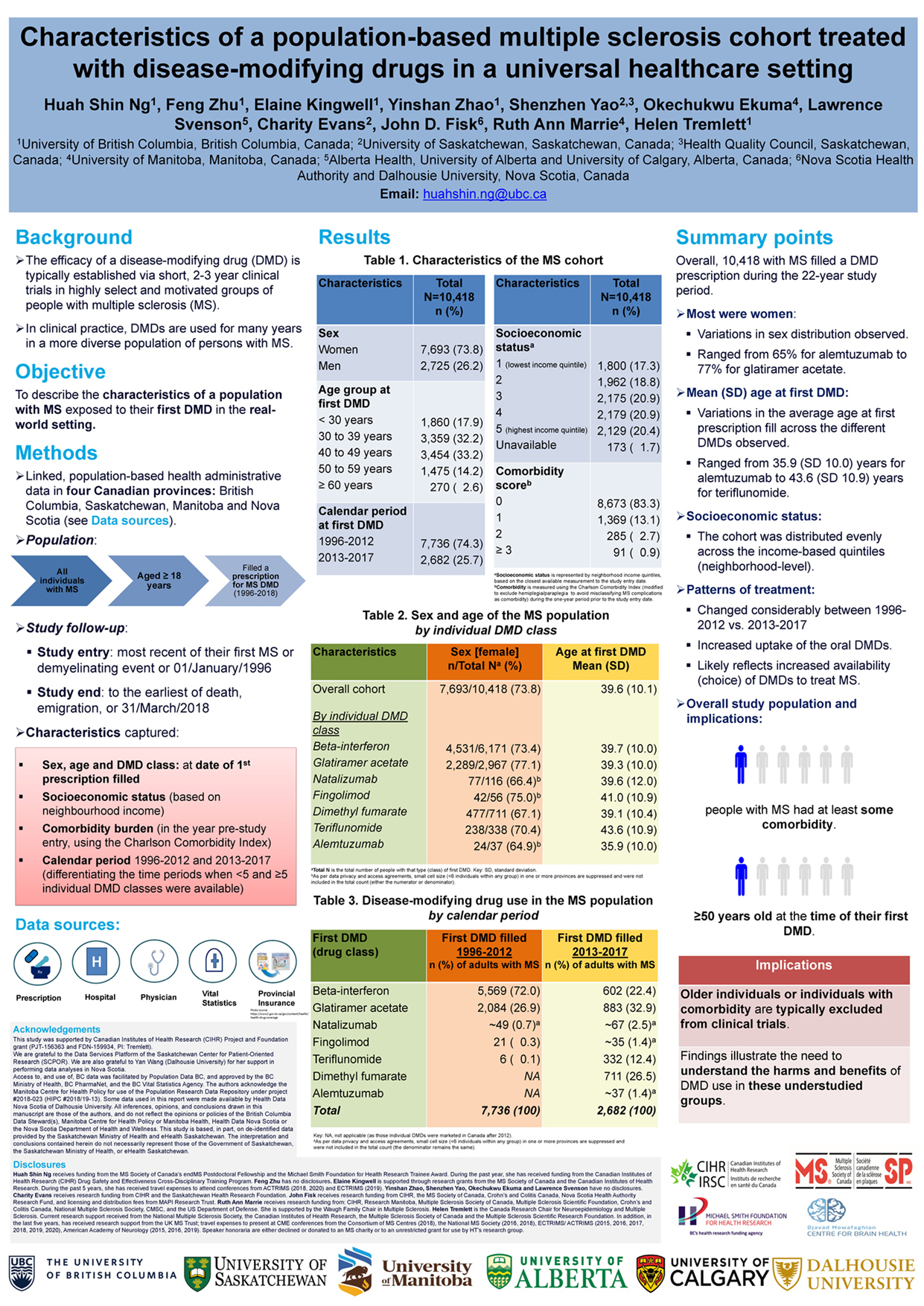
Overall, 10,418 of MS cases filled a DMD prescription during the 22-year study period. Most were women (n=7,683;74%), and the number of individuals was distributed evenly across the neighbourhood income quintiles. Seventeen percent (n=1,745) had some comorbidity (Charlson Comorbidity Index score ≥1) at study entry. Nearly 20% (n=1,745) were aged ≥50 years when filling their first DMD and 3% (n=270) were ≥60 years old. The mean age at first DMD prescription ranged from 35.9 years for alemtuzumab (n=43) to 43.6 years for teriflunomide (n=338). From 1996-2012, the most common first DMD prescriptions filled were for beta-interferon (n=5,569/7,736; 72% of people) or glatiramer acetate (n=2,084/7,736; 27% of people). From 2013-2017/18, the most common first DMD prescriptions filled were for glatiramer acetate (n=883/2,682; 33% of people) or dimethyl fumarate (n=711/2,682; 27% of people).
Conclusions:
Almost 1 in 5 people with MS had at least some comorbidity, and nearly 1 in 5 were ≥50 years old at the time of their first DMD. As these individuals are typically excluded from clinical trials, findings illustrate the need to understand the harms and benefits of DMD use in these understudied groups.
Characteristics of a population-based multiple sclerosis cohort treated with disease-modifying drugs in a universal healthcare setting
Huah Shin Ng, PhD,1 Feng Zhu, MSc,1 Elaine Kingwell, PhD,1 Yinshan Zhao, PhD,1 Shenzhen Yao, MSc,2,3 Okechukwu Ekuma, MSc,4 Lawrence W Svenson, PhD,5,6,7 Charity Evans, PhD,2 John D. Fisk, PhD,8 Ruth Ann Marrie, MD, PhD,9 Helen Tremlett, PhD1
1Department of Medicine, Division of Neurology and the Djavad Mowafaghian Centre for Brain Health, University of British Columbia, Vancouver, BC, Canada
2College of Pharmacy and Nutrition, University of Saskatchewan, Saskatoon, SK, Canada
3Health Quality Council, Saskatoon, SK, Canada
4Department of Community Health Sciences, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
5Alberta Health, Edmonton, AB, Canada
6Division of Preventive Medicine & School of Public Health, University of Alberta, Edmonton, AB, Canada
7Community Health Sciences, Cumming School of Medicine, University of Calgary, Calgary, AB, Canada
8Nova Scotia Health Authority and the Departments of Psychiatry, Psychology and Neuroscience, and Medicine, Dalhousie University, Halifax, NS, Canada
9Departments of Internal Medicine and Community Health Sciences, Max Rady College of Medicine, Rady Faculty of Health Sciences, University of Manitoba, Winnipeg, MB, Canada
Acknowledgements
Funding: Canadian Institutes of Health Research (CIHR) Project and Foundation grant (PJT-156363 and FDN-159934, PI: Tremlett).
We are grateful to the Data Services Platform of the Saskatchewan Center for Patient-Oriented Research (SCPOR). We are also grateful to Yan Wang (Dalhousie University) for her support in performing data analyses in Nova Scotia.
Access to, and use of, BC data was facilitated by Population Data BC, and approved by the BC Ministry of Health, BC PharmaNet, and the BC Vital Statistics Agency. The authors acknowledge the Manitoba Centre for Health Policy for use of the Population Research Data Repository under project #2018-023 (HIPC #2018/19-13). Some data used in this report were made available by Health Data Nova Scotia of Dalhousie University. All inferences, opinions, and conclusions drawn in this manuscript are those of the authors, and do not reflect the opinions or policies of the British Columbia Data Steward(s), Manitoba Centre for Health Policy or Manitoba Health, Health Data Nova Scotia or the Nova Scotia Department of Health and Wellness. This study is based, in part, on de-identified data provided by the Saskatchewan Ministry of Health and eHealth Saskatchewan. The interpretation and conclusions contained herein do not necessarily represent those of the Government of Saskatchewan, the Saskatchewan Ministry of Health, or eHealth Saskatchewan.