Intravenous immunoglobulin for acute attacks in neuromyelitis optica spectrum disorders
Abstract
Background:
Intravenous immunoglobulin (IVIG) has been used for therapy in a number of autoimmune disorders with various efficacy. This study aimed to investigate the efficacy of IVIG for patients with neuromyelitis optica spectrum disorder (NMOSD) during acute attacks.
Methods:
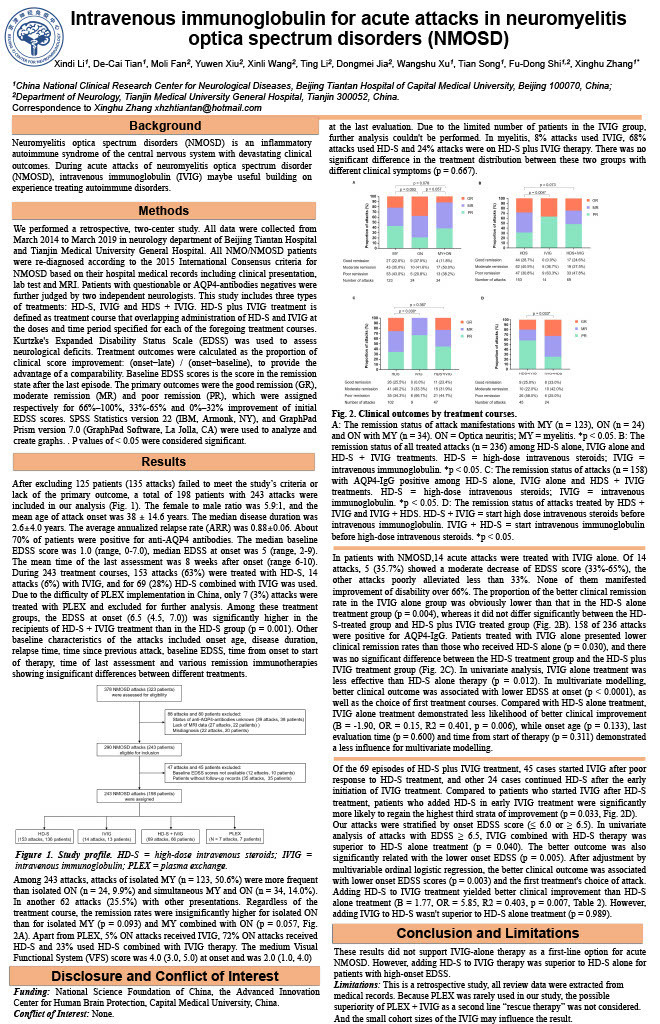
We retrospectively studied the treatment effects of several therapeutic strategies for NMOSD attacks at Beijing Tiantan Hospital and Tianjin Medical University General Hospital. Clinical outcomes were evaluated by the short-term remission status, which was categorized as good (GR), moderate (MR) or poor remission (PR) respectively based on the change of Expanded Disability Status Scale (EDSS) score.
Results:
A total of 243 attacks was analyzed in 198 patients from 2014 to 2019, among which153 attacks were treated with high-dose intravenous steroids (HD-S), 14 were treated with IVIG, 69 with episodes of IVIG plus HD-S, and 7 treated with plasma exchange. The proportion of patients with better outcomes were significantly lower in IVIG alone group than HD-S alone group (p = 0.004). However, sequential treatments by IVIG and followed HD-S yielded a higher likelihood of clinical improvement in severe attacks with EDSS ≥ 6.5 (OR = 5.85, p = 0.007).
Conclusion:
These results did not support IVIG-alone therapy as a first-line option for acute attacks of NMOSD. However, addition of HD-S to IVIG therapy may be superior to HD-S alone for NMOSD patients with high-onset EDSS.