A systematic review and meta-analysis of the prevalence of multiple sclerosis in patients with uveitis and characterisation of the phenotype of patients with both conditions
Abstract
Background:
Uveitis describes intraocular inflammation of the uveal tract. An association with multiple sclerosis (MS) has been observed. It is increasingly important to better characterise this relationship, as anti-tumour necrosis factor alpha (anti-TNFα) monoclonal antibodies are being used to treat refractory uveitis yet are known to cause incident demyelination and increase risk of MS relapse.
Methods:
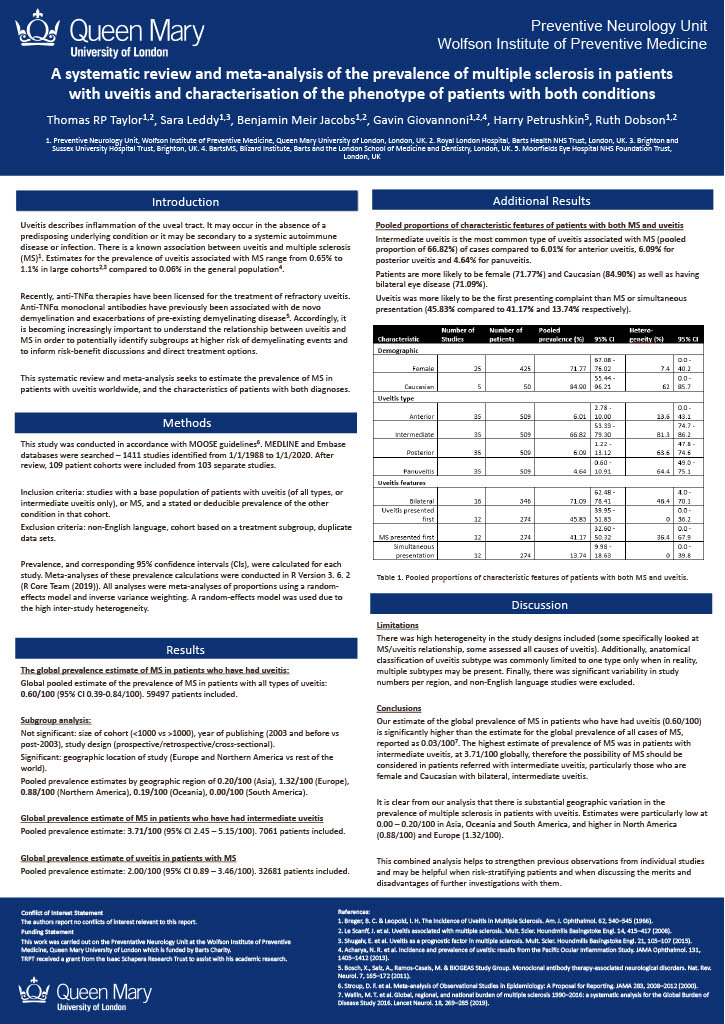
A systematic review and meta-analysis was undertaken to estimate the prevalence of MS in patients with uveitis and the characteristics of patients with both diagnoses. The prevalence of MS in the subgroup of patients with intermediate uveitis, and the prevalence of uveitis in patients with MS were also estimated. Medline and EMBASE databases were searched from 1/1/1988 to 1/1/2020, yielding 109 patient cohorts from 103 studies. A meta-analysis of proportions using a random-effects model was performed. Heterogeneity was analysed using meta-regression and subgroup analysis.
Results:
The overall pooled prevalence of MS in uveitis was 0.60/100 (95% CI 0.39-0.84/100). There was significant geographic variation, with the highest prevalence seen in North America (0.88/100) and Europe (1.32/100). Patients with dual diagnoses were most likely to be female and Caucasian with bilateral, intermediate uveitis.
Conclusions:
This study confirms an association between MS and uveitis and identifies the characteristics of those most commonly affected. This may help to plan future prospective studies into the relationship between these two diseases, and can inform discussions in those patients with uveitis who are at the highest risk of developing MS.