Anterior optic pathway pathology in CNS demyelinating diseases
Abstract
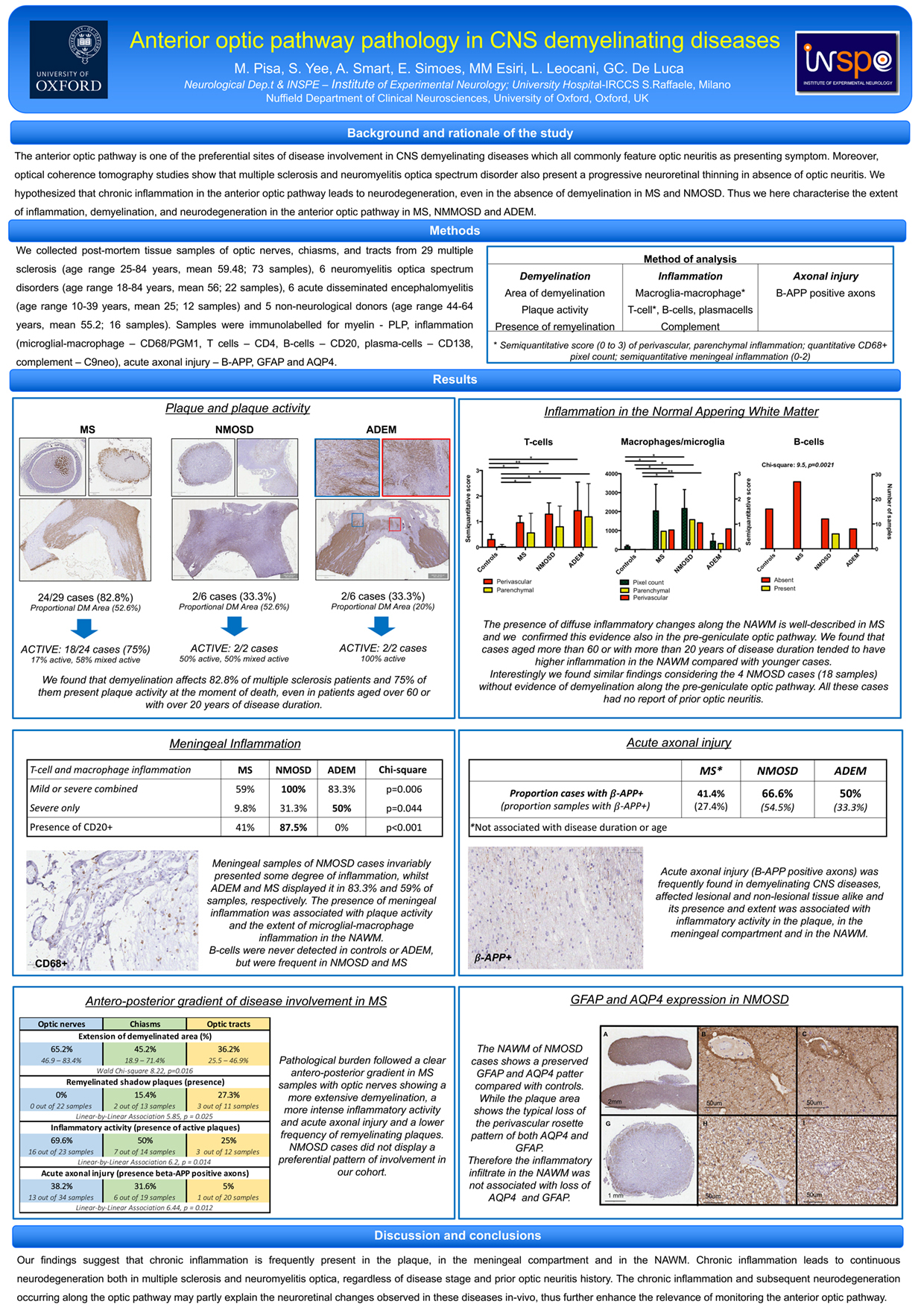
The anterior optic pathway is one of the preferential sites of disease involvement in CNS demyelinating diseases which all commonly feature optic neuritis as presenting symptom. Moreover, optical coherence tomography studies show that multiple sclerosis and neuromyelitis optica spectrum disorder also present a progressive neuroretinal thinning in absence of optic neuritis. These recent evidence point to the need to reassess the pathological characteristics of this relevant CNS area.
We collected post-mortem tissue samples of optic nerves, chiasms, and tracts from 29 multiple sclerosis (age range 25-84 years, mean 59.48; 73 samples), 6 neuromyelitis optica spectrum disorders (age range 18-84 years, mean 56; 22 samples), 6 acute disseminated encephalomyelitis (age range 10-39 years, mean 25; 12 samples) and 5 non-neurological donors (age range 44-64 years, mean 55.2; 16 samples). Samples were immunolabelled for myelin, inflammation (microglial-macrophage, T and B-cells, plasma-cells, complement), acute axonal injury, GFAP and AQP4. We found that demyelination affects 82.8% of multiple sclerosis patients and 75% of them present plaque activity at the moment of death, even in patients aged over 60 or with over 20 years of disease duration. Moreover, microglia-macrophage and lymphocyte inflammation are frequently found both in the meningeal compartment and the normal appearing white matter. Acute axonal injury was detected in 41.4% of donors, its presence and extent are correlated with the intensity of the inflammatory activity in each compartment. Interestingly, inflammation does not equally affect the optic pathway but shows a clear antero-posterior gradient with optic nerves being most severely affected, whilst the optic tract display a higher proportion of remyelinated plaques, suggesting an inverse relationship between inflammation and remyelination. In neuromyelitis optica spectrum disorder cases with prior optic neuritis history, demyelination was extensive and associated with loss of the typical GFAP and AQP4 perivascular rim. Instead, donors who never experienced optic neuritis did not present demyelination along the optic pathway but showed diffuse microglial-macrophage, T and B-lymphocyte inflammation in the normal appearing white matter, invariably presented meningeal inflammation and had evidence of acute axonal injury in 75% of cases. Acute demyelinating encephalomyelitis featured intense inflammation and perivenular demyelination.
Our findings suggest that chronic inflammation is frequent and leads to neurodegeneration in multiple sclerosis and neuromyelitis optica, regardless of disease stage and prior optic neuritis history. The chronic inflammation and subsequent neurodegeneration occurring along the optic pathway may partly explain the progressive neuroretinal changes observed in these diseases in-vivo.