Subclinical anterior optic pathway involvement in early multiple sclerosis and clinically isolated syndromes
Abstract
Optical coherence tomography is gaining increasing relevance in the assessment of people with multiple sclerosis. Converging evidence point to the view that neuro-retinal changes, in eyes without acute optic neuritis, reflect inflammatory and neurodegenerative processes taking place throughout the CNS.
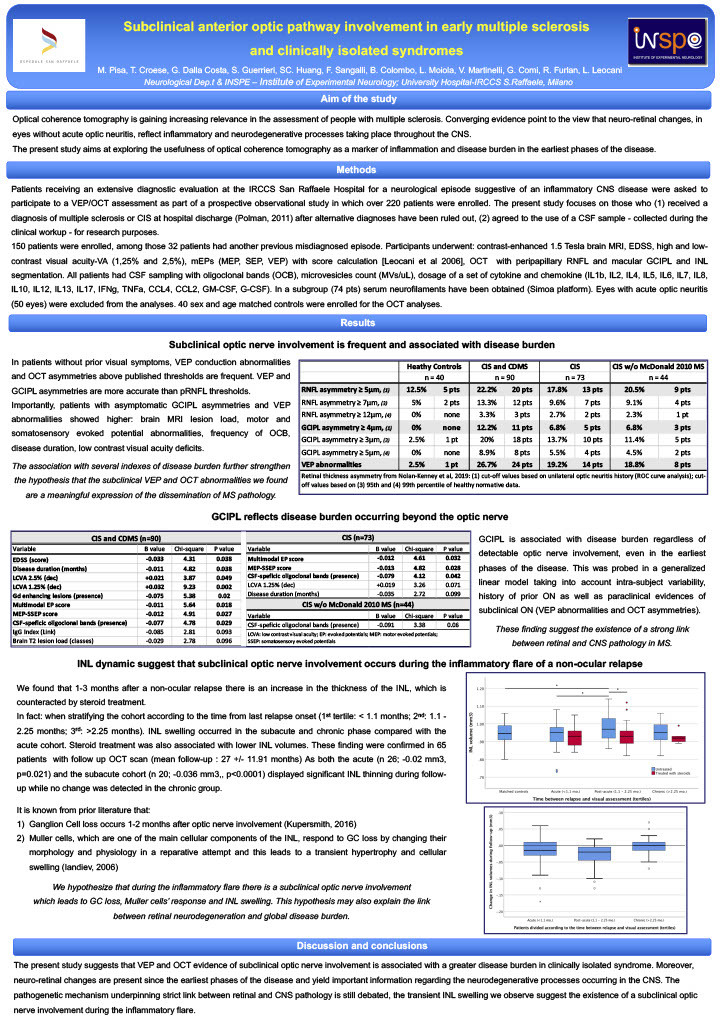
The present study aims at exploring the usefulness of optical coherence tomography as a marker of inflammation and disease burden in the earliest phases of the disease. Thus, a cohort of 150 consecutive patients underwent clinical, neurophysiological and brain MRI assessment as well as lumbar puncture as part of their diagnostic workup for a neurological episode suggestive of inflammatory CNS disorder; among those 32 patients had another previous misdiagnosed episode. For the present study, patients also received a visual pathway assessment (optical coherence tomography, visual evoked potentials, visual acuity), measurement of CSF inflammatory markers (17 cytokines-chemokines, extracellular vesicles of myeloid origin), and dosage of plasma neurofilaments.
Subclinical optic nerve involvement is frequently found in clinically isolated syndromes by visual evoked potentials (19.2%). Optical coherence tomography reveals ganglion cell layer asymmetries in 6.8% of patients; retinal fiber layer asymmetries, despite more frequent (17.8%), displays poor specificity. The presence of subclinical involvement is associated with a greater disease burden. Second, ganglion cell layer thinning reflects the severity of disease involvement even beyond the anterior optic pathway. In fact, ganglion cell layer in eyes without evidences of subclinical optic involvement is correlated with EDSS, low contrast visual acuity, disease duration, brain lesion load, presence of gadolinium enhancing lesions, abnormalities along motor and somatosensory evoked potentials, and frequency of CSF-specific oligoclonal bands.
Third, inner nuclear layer thickens in a post-acute (1.1 – 3.7 months) phase after a relapse, and this phenomenon is counteracted by steroid treatment. Likewise, a longitudinal analysis on 65 patients, shows that this swelling is transient and returns to normal values after one year of follow-up. Notwithstanding, the clinical, MRI, serological and CSF markers of disease activity considered in the study are strictly associated with one-another but none of them is associated with inner nuclear layer. Our findings challenge the current hypothesis that inner nuclear layer is an acute phase marker of inflammatory activity.
The present study suggests that instrumental evidence of subclinical optic nerve involvement is associated with a greater disease burden in clinically isolated syndrome. Neuro-retinal changes are present since the earliest phases of the disease and yield important information regarding the neurodegenerative and inflammatory processes occurring in the CNS.